Telehealth in Europe is boosting. More and more patients are having online consultations with their GP or health professional and digital services are claiming a permanent place in the healthcare system. ‘Thanks’ to the global Covid-19 pandemic, several national governments saw the growing need for the reimbursement of teleconsultations and put a legislation in place. By doing so, they added teleconsults to the set of commodity health services.
But did you know that in some European countries the shift towards digital health innovation took place way before we had even heard of the coronavirus? These are Europe’s telehealth-frontrunners and France is definitely one of them.
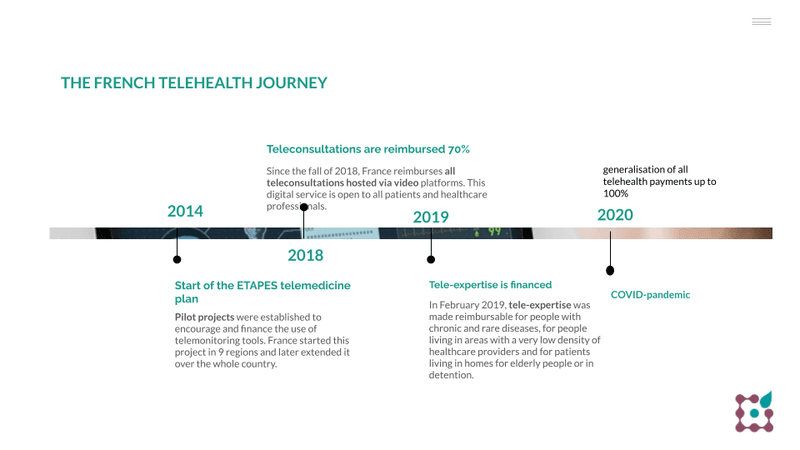
This timeline shows the country started its health innovation journey in 2014 and kept evolving over the following years.
Thanks to the straightforward choice of the French government, telehealth is now broadly implemented. Both patients and physicians have easy access and are used to teleconsultations, as a stand-alone solution or as a part of the telemedicine process of diagnosis, monitoring and therapy.
Which other European countries recognised the benefits of digital healthcare early on and now have a large, well-functioning telehealth industry?
- The Nordics: the first Danish action plan for telemedicine was established in 2012. In 2016, Swedish doctors became available for video consults via smart phone apps.
- Estonia: Estonia had a national eHealth Foundation since 2005. Four years later, physicians started to store patient’s health data on large scale. In just a few minutes, this information can be exchanged between hospitals or other healthcare professionals.
- The United Kingdom: the National Insurance provides free telemedicine when it is administered by an authorised physician. Telehealth is included in most private health insurances as well.
- Germany: since 2018, physicians can host teleconsults without alternating them with face-to-face consultations.
Curious to find out more about digital health in Europe? Then become a member of the dashplus community and receive our free twoweekly newsletter or take a look at our brand new ebook.
- Join our Community
Why do the French believe in telemedicine?
L’Assurance de Maladie, the French Health Insurance organisation, sees telemedicine as a way to improve overall healthcare and to make it more accessible to all French citizens.
The national Health Insurance acknowledges that teleconsultations offers several benefits, such as:
- People living in remote areas get easier access to specialised healthcare professionals
- Treatment and follow-up can be administered faster as waiting times decrease
- Unnecessary visits to hospital’s emergency departments can be avoided
- Cooperation between different healthcare professionals gets easier. They can ask for each other’s advice and share their expertise. This improves their knowledge and their ability to treat patients
Already in 2018, rules on how to administer a teleconsult, what to charge for it and how to reimburse it were created during a national medical convention.
This is how teleconsultations in France are organised since 2018:
Principle 1: open to all patients and all health professionals
It includes all patients and all doctors. All patients have access to teleconsultations: young and old people, wherever you live, and regardless of your medical history. All doctors can deliver the service: GP’s as well as specialists, no matter if they work in a private practice, a hospital or other medical centre.
The French government and the French High Council of Health explicitly choose to make digital consultations accessible for everyone.
This is an important guide for other countries implementing digital health services in their system, since:
- the principle of accessible healthcare to everyone is key in Europe
- patient freedom to choose their health professional is also key within Bismarck systems in Europe
- digital consultations, in general, enhance access to healthcare services, so it is contra-intuitive to make this selective for certain patients and health professionals
Principle 2: the doctor guides to a teleconsultation
Teleconsultations are not meant to replace physical consults. In some cases, they are not the best answer to a patient’s needs. This decision has to be made by the health professional delivering the teleconsultation service.
Telemedicine in France should be part of a coordinated health plan. Moreover, the patient using the teleconsultation service should be known to the physician who delivers the service. This means patients ought to have had a physical consultation with the doctor no longer than 12 months ago.
However, exceptions to this principle make it possible for both patient and physician to use teleconsultations more flexible. The previous patient-doctor relation is not necessary for/when:
- children up to 16 years old
- patients having no permanent personal GP (or GMD)
- highly-wanted specialist doctors
- the regular doctor is unavailable (for example: during weekends or late in the evening)
- circumstances are urgent
Principle 3: teleconsultations are video-based and secured
The teleconsultation is hosted via a secured, video-based platform on laptop, smartphone or tablet and guarantees the security and privacy of the patient and the healthcare professional. The platform features a summary of the consultation, a payment service, and an e-prescription service.
Also interesting: French law says an extra health or social professional is allowed to be present to help the patient during the teleconsultation. Which is useful for elderly people for example. Moreover, patients might be guided to teleconsultation contact points (service centres or pharmacies), to take measurements that support the physician’s diagnosis for example.
Principle 4: digital and physical consultations cost the same
Fees for teleconsultations and physical visits are the same. The cost lies between € 23 and € 58,50, depending on the type of specialism of the healthcare provider. Patients pay for teleconsultations online, with a cheque or by bank transfer. The French government refunds 70% of teleconsultation services and up to 100% for people with chronical conditions.
In July 2020, France decided to accelerate the implementation of telehealth even more by: a 100% reimbursement (instead of 70%), for all teleconsultations and including new HCP like pharmacists, speech therapists, midwives, nurses and physiotherapists. Previously, also Belgium adopted this kind of rules at the beginning of the first lockdown.
User profiles and their opinion on telehealth
Since 2018, since the start of the general financing of teleconsultations, usage numbers did steadily increase. We noted an average of 4.000 to 5.000 a week.
But the covid-beast had a gigantic impact on the use of telehealth. In February 2020, 40.000 teleconsultations administered by more than 3.000 physicians, were reimbursed in just one week. And that number peaked to
approximately 1 million teleconsults by the end of March 2020.
Of course, this was due to sanitary measurements, but also telehealth regulations were made more flexible:
- it was no longer necessary that a physician already knew his/her patient before suggesting a teleconsult
- a remote consult could be hosted over the phone as well, where previously all teleconsults had to be held over a secured video platform
- teleconsults were 100% reimbursed during the pandemic (compared to a reimbursement between 70 and 100% before) and so were telesurveillances administered by nurses
So the successful use of telehealth in France was made possible thanks to the large, mature legislation and reimbursement system that existed already when COVID got hold of Europe. A swift and flexible adoption was possible, both by patients as well as doctors, since seeds were planted already years before. And these were present in public policy, but also in the startup ecosystem.
Thus, it’s not entirely unexpected that Sifted, the European startup-blog of Financial Times, recently speaks of the ‘French tech revolution’: France is a frontrunner in telehealth, but also in other tech sectors.
Did you know that our blog has readers from all countries that are considered to be Europe’s frontrunners? You can easily join this community too:
OR: join one of our masterminds on telehealth here!
Is telehealth only for the young hipsters?
Telehealth is often said to be a service that doesn’t reach older people. Criticasters believe that the physicians and patients using teleconsults are to be found amongst the young hipsters. But is that true?
On the doctor’s side, data show 27% of all teleconsultations in France are delivered by physicians over 60 years old. This is in line with the representation of this age group within the whole French HCP-population.
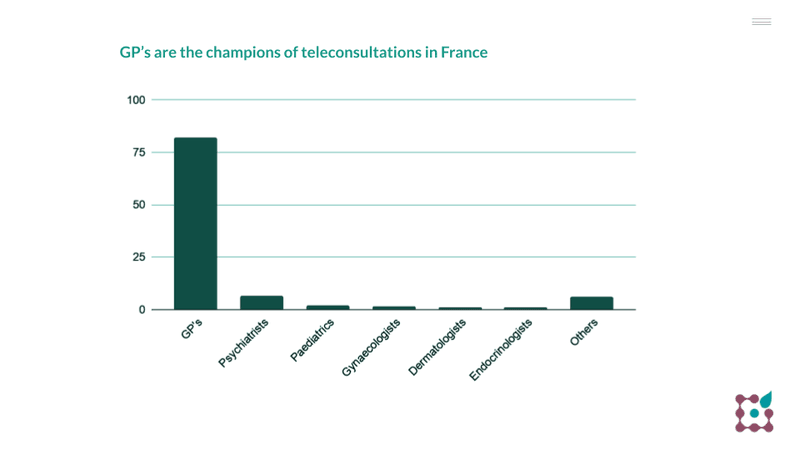
General practitioners are the champions of teleconsultations in France: approximately 80% of all teleconsults are administered by them. Other HCP frequently using virtual consultations are: psychiatrists, paediatrics, gynaecologists, dermatologists and endocrinologists.
On the patient’s side we notice a shift towards older patient groups since covid19. Traditionally, teleconsultations were very popular among urban thirthy- and forty-somethings. Since covid, users aged 50 plus grow rapidly, with 20% aged 70 and older (coming from only 8% in 2019). And during the lockdown, telehealth also became ‘normal’ for people living in smaller cities and villages.
People with chronic diseases count for 23-28% of all teleconsultations.
- Don't miss any innovations in healthcare
What do patients and physicians think about telehealth?
Now that telemedicine usage is skyrocketing, it is the ideal time to take a look at the satisfaction rates. The national agency ANS questions citizens and physicians each year. Early 2021, they interrogated about 3.000 patients and 500 healthcare professionals.
This public barometer on teleconsultations indicates:
- French citizens are getting to know telehealth. And they are convinced it has a positive impact on national health.
- 73% of the national population is in favour of teleconsults. This is one of the highest rates in Europe.
- Physicians having used teleconsultations once, keep on using it. On average, they administer 91 virtual visits a year.
- French patients give a satisfaction rate of 88%; 8% higher than the average European score.
- Healthcare professionals that have hosted teleconsultations, award it with a satisfaction score of 78%.
- 70% of the French population is willing to book a teleconsultation if their GP or healthcare provider proposes it.
To me this illustrates the famous quote of J. Goodwin in society:
The impossible is often the untried.
La French healthcare tech
Telehealth regulations in France no doubt are a blessing to the market size and cost saving opportunities in the country, also indicated by our colleagues of Research2guidance. And we already talked about the social and cultural impact of it. But no doubt, they also have a favorable impact on the French healthcare business ecosystem. From startups to corporates, French as well as international companies, are building telehealth services in la douce France. And this, in turn, will spark startups and ventures in other healthcare-segments in France.
Here are 3 of the most important teleconsultation platforms in France:
- Doctolib is one of the three most used digital health tools on the international scene. It offers a fully integrated teleconsultation service equipment to physicians and other HCP, making it possible for them to gain quality of life and comfort too. Worldwide, it has over 35 million users now.
- Livi is the brand of Swedish teleconsultation pioneer KRY in France. It’s on a mission to make care accessible to everyone. Livi hosts more than 3 million consultations in Europe on a yearly basis and is active seven days a week. Both children and adults connect with healthcare professionals in different disciplines through the platform.
- Medaviz is a platform that offers teleconsultation and tele-expertise. Different from Livi and Doctolib, its main entry point is the doctor rather than the individual patient. Medaviz hosts more than 400.000 consultations and connects 9.000 healthcare providers in 50 disciplines, 24 hours each day.
Over 10 teleconsultation platforms are now active in the French market. Check out some more in our blog ‘visit your doctor online? This is how it’s arranged in France’ from 2019.
How does the future look like?
1. France wants teleconsults to become a ‘normal’ way of providing health services. Teleconsults need to become a sustainable option for French patients according to the government. A mission that looks like it’s going to succeed.
Although experts expect that the current teleconsultation usage numbers will still decline somewhat, now that a lot of hospitals and GP’s are returning to their usual way of functioning. We know that in mature systems like the Nordics and France, teleconsultations can make up 10-15% of all doctor’s visits after 4 years.
2. The proximity aspect: in ‘Ma Santé 2022’, the French government sketches the wish for proximity in future health: all citizens need to have sufficient access to healthcare providers and specialists.
That’s why France started labelling ‘proximity hospitals’. By 2022, the country aims to have 500 to 600 facilities were general medicine, care for the elderly, follow-up and rehabilitation care, specialty consultations and non-medical consultations are provided. These proximity hospitals must have sufficient telemedicine equipment. So the deployment of telemedicine and telemonitoring in hospitals will further grow.
3. Digital healthcare innovation asks for financial investments. Hospitals and other HC organisations will need to invest more in digital health. France has an open economy and allows large private initiatives to invest in healthcare companies. Thanks to the rapid shift towards digital healthcare that is currently going on, telehealth initiatives and start-ups are seen as interesting businesses to invest in. Take Doctolib for example: the app was launched in 2013 and raised € 237 million since then. A part of that money was contributed by physicians and healthcare providers who pay to use Doctolib’s services and who may contribute to the further development of the platform in return.
It’s a combination that creates beautiful opportunities for ‘la French healthcare’. So, the future looks bright. And isn’t this a perspective we all want in Europe?
Good to know: In Belgium, private insurance company AXA started its telehealth service to over 500.000 insurance clients in 2019. An initiative dashplus was happy to guide along.
Do you want to know what dashplus can do for you? Send us an email or give us a call. We’ll gladly help you implementing digital innovation into your business.
- Join our Community










