Digital consultations will be financed in the Belgian health system as of 1 August 2022. This way the country at the heart of Europe follows the worldwide trend to include telehealth and to prepare hybrid care delivery.
Although this is a step forward, there are still some challenges for Belgium to be a European frontrunner in telehealth. Accessibility to telehealth services is one of them.
This is striking. Especially since digital consultations are helping weaker groups to find health care:
- various studies show that more than 80% of Belgians are digitally active on a daily basis
- And that 77% of people with a lower socioeconomic status consider their computer or smartphone indispensable.
- In the US, telehealth has helped these people especially during COVID.
- In France, figures from teleconsultation platform Doctolib show that the majority of their users live in small rural towns or in larger cities.
- in Belgium, after one year, the Proximus Doktr app is noticing more than 10% of users aged 70 or over.
- Telehealth also reduced non-attendency in primary care with over 20%, a study of Drerup mentions. And we know no-show rates for health care are especially high for male patients and patients with lower SES.
Not all Belgians will have equal access to digital consultations
Unfortunately, access to care is being challenged by the new regulation: there is a risk that not all Belgians will have equal access to reimbursed digital consultations.
Why?
- if you do not have a GMD-physician (traditionally more young people and/or people of foreign origin are in this case) or
- you didn’t visit the specific GP in the last 2 years physically (e.g. because you have moved, or because you were not ill),
then health administration RIZIV/Inami will not reimburse a digital consultation for you.
This means you will need to pay 100% out of pocket or via a private insurance.
At the moment, this concerns at least 2.8 million Belgians.
Also people who live in areas with GP shortage are at risk of losing out: they have to deal with patient stops and not finding a GP in time. Next, using telehealth to receive medical help, they will have to pay it fully private.
And there are other examples: what if I am on holiday and I want to see a doctor, for example, at the seaside? Or I need a specialist for which there is a long waiting time, e.g. a dermatologist. Tom Braekeleers has mentioned this problem too in his nice column on the new telehealth-arrangement.
Want to discuss on telehealth with others in the health ecosystem? Join the mastermind group telehealth
Financing for other healthcare providers and specialists
Next, it’s also very unfortunate a lot of care providers have no perspective on telehealth financing yet: what about speech therapists, psychologists, physiotherapists and dentists, for example?
And what about specialists? The fee for a video consultation for GP’s is the same as for a physical consultation, so that's okay. But for doctors-specialists, the incentive is limited: digital consultations are sometimes valued half of a physical consultation…
In times of high infrastructure costs, maintenance and mobility costs, this seems a missed opportunity for hospitals and for the government. They could have done more for specialists who want to combine patient centricity with work-life balance.
Other European countries like France, Germany, Portugal, … pay digital and physical consultations equally. It’s exactly how it should be, evolving to hybrid care. Professional organisations of specialists have a role in this.
Training and technical
A third challenge, next to accessibility and equal payment, is telehealth education and training for healthcare professionals. They indicate that they know too little about digital possibilities and that they receive insufficient training during medical school: more than 78% of doctors have this opinion, according to a current master's thesis at the VUB university.
So, there’s still a journey to make in Belgium. Let’s start by not seeing digital consultations as a ‘threat’ to social contact, but as an enrichment of contact points with patients.
Last but not least, there’s the importance of a transparant technical level-playing field. Many specialised platforms and apps for digital consultations are active in Europe: about 10 in France, 4 in Portugal, 5 in Finland… . These countries already have technical criteria and assesments in place. European or worldwide standards make sure all companies are treated in the same way.
- Join +2000 health innovators
The future is hybrid
Hybrid healthcare models will be the way to go.
And these 3 steps are needed in Belgium now:
- learning about the real-life application of digital consultations. Sharing insights, experiences and lessons of both patients and medical professionals. Doing and adapting along the way
- an arrangement for tele-expertise
- a generic public financing of mobile health apps, starting from the sandbox model
Read all about telehealth financing in Belgium
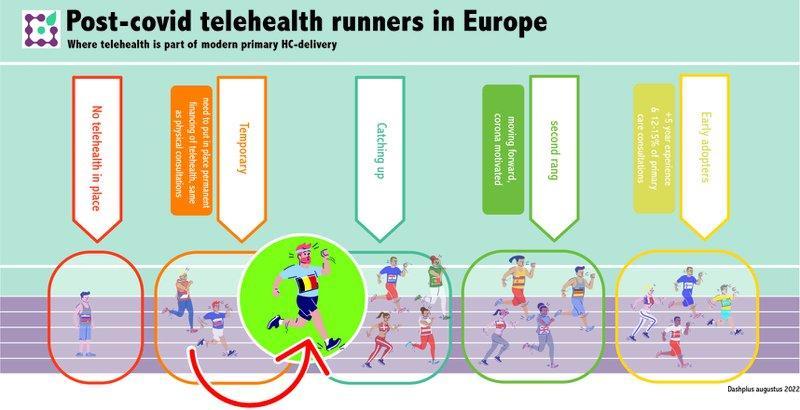
Check out how telehealth is organised in Europe
Contact us to answer your specific questions










