Telehealth is healthcare delivery at a distance, via digital technology channels (telephone or video). In Europe, telehealth and telemedicine are often used interchangeably. Virtual consultations or teleconsultations involve at least a patient and an HCP, while tele-expertise refers to digital consultations of HCP with peers.
Since covid, telehealth has proven to be a great help in providing (primary) care all over the world. At the start of the pandemic, the WHO called for action and the widespread use of telehealth.
European countries that had already introduced digital consultations to the public health system benefited from it: for them, the changeover was quicker and easier to make. Their doctors and their citizens were already more familiar with digital healthcare.
A huge real-life learning experience for governments
COVID was a huge learning experience in the real-life application of digital consultations: an unprecedented amount of research, surveys and insights were published that teach us a lot about HC delivery, practice organization and the outcome of telehealth in the year 2021. To illustrate: Google Scholar shows 10,6k results for ‘telehealth outcome Europe’ since 2020 and 8640 for ‘healthcare delivery telehealth’ in 2021 alone.
Smart governments immediately reaped the benefits. France and Germany, for example, have removed some of the restrictions that initially existed on digital consultations. Others, such as Belgium, are on the eve of a permanent implementation in the public health system.
Everyone agrees by now: telehealth is here to stay and is part of modern, hybrid healthcare service. Telehealth is not a replacement for physical consultations, but it is an equally valuable channel that will offer numerous exciting possibilities to healthcare professionals and citizens: it enables new relationships, new practices and value-based healthcare.
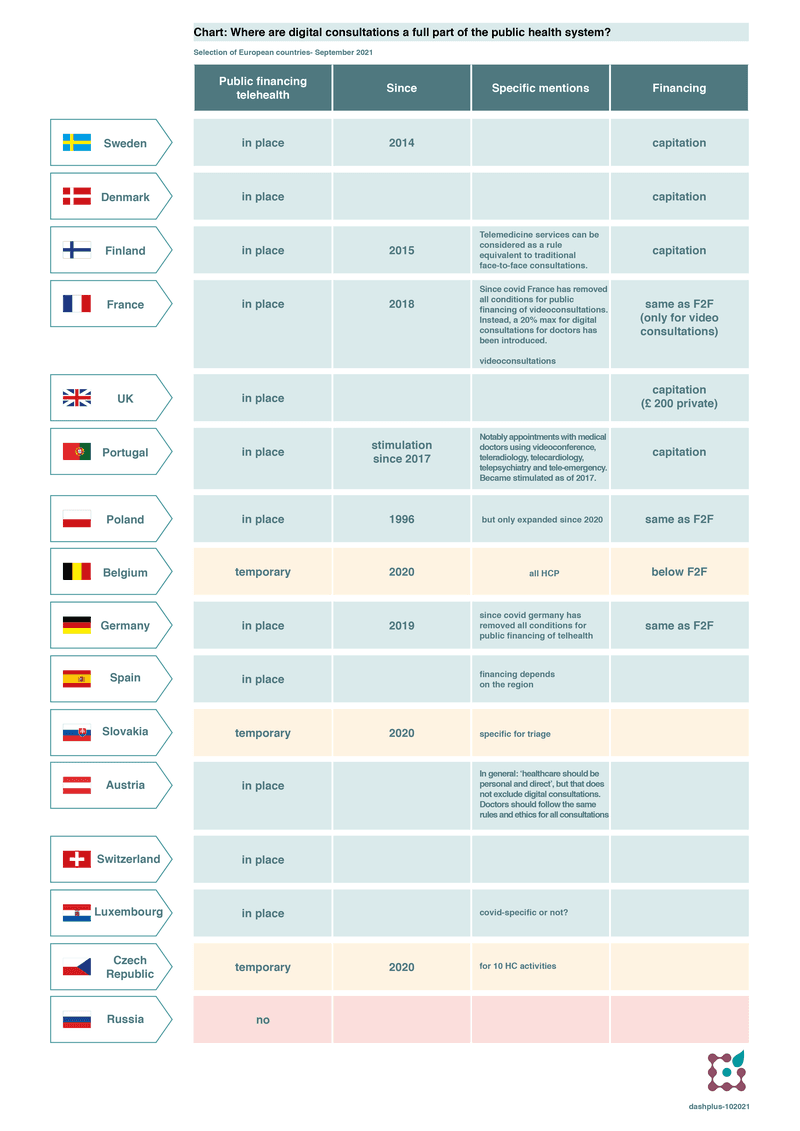
But what exactly is the situation in Europe post-covid? What public health systems reimburse digital consultations? How do European countries organise teleconsultations post-covid? And what do Slovakia, Czech Republic and Belgium have in common?
4 things you should know about telehealth in Europe post-covid
We have made an overview of the rules in several European countries in September 2021 (so more or less post-covid) and have come to 4 striking conclusions:
1) Teleconsultations are a fully-fledged and permanent part of the public health system in most European countries
Most European countries have already introduced digital consultations as a fully-fledged permanent part of the public health system: it follows the same rules, the same fee and the same reimbursement as physical consultations.
In most cases, there is also an explicit statement that telehealth is an equivalent form of health service. Moreover, some governments state that doctors need to announce their digital services publicly e.g. by posting them in the practice or on the website. This guideline has been explicitly adopted in Poland and Luxembourg, for example.
However, such permanent inclusion in the public health system is NOT yet the case in Belgium, the Czech Republic and Slovakia: here the arrangements are still temporary and in relation to covid. In Spain and Finland, there may be differences between regions as they have responsibility for telehealth. But both countries are doing well overall.
CHART: Where are digital consultations a full part of the public health system? Selection of European countries-September 2021
2) Most frequently used in primary healthcare
In all countries, teleconsultation is most frequently used by general practitioners (GP’s), psychologists, speech therapists and dentists.
They do so via specialized communication platforms that are specifically equipped for telehealth and guarantee:
- GDPR and security standards;
- good picture quality;
- smooth and evidence-based triage;
- an easy-to-use tool for the entire process and;
- support for questions or problems.
In countries where the government has developed its teleconsultation platform (as in Luxembourg), this is optional. So both doctors and patients are free to choose the channel through which they contact each other.
In countries like Sweden, Denmark and Finland, which were pioneers of digital health in Europe, 12% of all medical consultations are now conducted via video (this is after 5 years on average).
3) Telehealth in Europe quality: guidelines and video consultations
The quality of digital consultations is just as important as that of physical consultations. That’s why most European systems define minimum quality requirements in explanatory notes or guidelines. These include typically some provisions on the privacy and security of the consultation, information that must be available to the doctor and that he/she must include in the patient’s medical file, and on the doctor’s therapeutic freedom. These guidelines are no different from those for ‘classical’ consultations.
Furthermore, in the context of quality and avoiding possible overconsumption (a fear in specifically fee-for-service systems), France and Germany only finance video consultations. It is indeed evident that quality is much better when a patient and a doctor can actually see each other instead of just talk to each other by phone.
4) No more quantitative limits
Whereas previously there were still limits on the number of digital consultations for which physicians were reimbursed, this has almost disappeared in post-covid time. Only France now applies a global 20-80% rule for all consultations. While Germany already scrapped this rule in the autumn of 2020.
It’s also important to note that the original quantitative limitations in these fee-for-service systems did not exclude patients from the digital option: people could use more digital consultations, but they had to pay a higher amount out-of-pocket in that case (e.g. at 30% reimbursement instead of 70% originally in France in 2019).
But as said, most countries make no difference between digital and physical HC-delivery: the same rules and principles apply to both. In Luxembourg, for example, the rule is 1 consultation/pp/day and the doctor is reimbursed – irrespective of whether this is a digital or physical consultation.
Conclusion
The covid-pandemic has led to real-life evidence about the readiness and outcome of telehealth in Europe. Healthcare systems that had already installed public financing of teleconsultations could move faster and opened up their regulations. Others, like Belgium and Slovakia, adopted temporary covid arrangements. They are on a point of permanent decision post-covid now.
Those countries can learn from their European neighbours in the Nordics, France and Germany where:
- HC systems explicitly state that telehealth is an equally valuable channel of HC-delivery
- HCP announce their digital service publicly to patients
- digital consultations follow the same quality rules and guidelines as other consultations
- out of quality reasons, video consultations are preferred
- there are no quantitative limitations to the financing of digital consultations different from physical consultations
- financing is at the same level or in a capitation-based system (as in the Nordics)
- the freedom of patients and HCP is respected
If you found this interesting: join our newsletter:
And stay on top of new articles on telehealth (it's two-weekly and FREE):