Healthcare expenses and care delivery in Finland
Finland is a relatively sparsely populated country with 5,5 million inhabitants. It has an ageing population with 25,6% being older than 65 years (1). This leads to an upward trend in the health expenditure per capita from 1800 million euro in 2000 to 3727 million euro from the year in 2017.
It is a vast country, with very remote areas and urban regions around Helsinki and Oulu.
Finland has a highly decentralized healthcare system based on public care providers. Primary care centres with multidisciplinary staffing are the main providers of primary care. Specialized care is provided by hospital districts. Municipalities, through taxes, finance most of the healthcare. The government is providing additional support. There are additional private services based on insurance and service fees. And medical centres contract private services.
Due to the economic crisis of the 1990s, Finland struggled with a shortage of health care workers: mainly GP’s and dentists. Many doctors studied and stayed abroad, and most norther-eastern communities suffered from this lack of accessibility. Although medical students doubled and the number of practising physicians increased by 28%, still 6% of all posts for doctors in medical centres stayed open in 2018.
On the other hand, the nurse-to-doctor ratio in Finland is one of the highest of the OECD countries: in 2014, there were 4,4 nurses for every doctor. ‘In 2018, nurse consultations covered 50% of the total number of non-urgent outpatient visits in health centres and they typically work in multidisciplinary teams or in pairs with physicians.’
Patients can choose what primary care centre to go to, but due to a ‘public tradition’ most people keep on going to the nearest one, although waiting times for primary care needs can be as long as one month (!). Indeed, public health centres keep on struggling to find enough physicians, and it seems like younger doctors prefer to work in private centres. The plans of the government to find 1000 extra physicians leads to a discussion: is the need for extra doctors a myth? The director of the innovation fund Sitra claims the contrary: efficiencies in the system and the system of private family doctors are enough to help Finland out.
All of these make Finland an interesting case to see how the combination of physical and digital healthcare-delivery (or hybrid care) will evolve. Especially since the country is a European pioneer of eHealth.
- Don't miss any innovations in healthcare
Basics in digital health since the nineties: tools, education and Kanta
Already in the mid-1990s Finnish government initiated a national strategy regarding the development and implementation of eHealth.
As a consequence, the Finnish Society for Telemedicine and eHealth (FSTeH) was founded in 1995. The first electronic tools for health professionals were developed in 2004. They included e-prescriptions, e-referrals and e-consultations. So Finland already has 17 years of experience now…
The investment in ICT education of Health Care (HC) professionals is another keystone. In 2012, Finland was the first country in Europe to establish a professional special competence for healthcare information technology to physicians. Medical professionals can follow approved theoretical studies and add 2 years of full time service in healthcare information technology positions. In 2016 already 58 physicians graduated.
And since 2014, Finland is supporting citizens to manage their own well-being by:
- improving health information management: data sharing and smart systems
- increasing online health services by the do-it-yourself principle
Kanta services, a common national health data information exchange platform was developed. The main components are patient data repository services, patient data management services and ePrescription services. It has a special interface, the My Kanta pages, giving all Finnish citizens secured digital access to his or her medical information.
So all of this this means basic infrastructure and tools are available since 2015 to scale digital health services. A report of the National Institute for Health and Welfare that year states Finland is well on the way towards digitizing many of the healthcare services. Prescriptions, laboratory test results and services booking are most frequently electronically used and needed by citizens.
Two decades of real-life experience with telemedicine
Also, Finland has gained extensive experience with telemedicine. Already in 1998, the Oulu University Hospital started video consultations for psychiatry. Simultaneously, orthopaedic teleconsultations started in Pori central hospital. In 2001 the Lapland County built a telemedicine consultation network between the central hospital in Rovaniemi and all the primary health centres in the region.
These and other applications were documented early on in academic research. There is wide research available on patient and doctors experiences, outcomes and costs. For example: first research in 2006 on the cost of a videoconsultation between a patient and a GP in a remote area with a specialist elsewhere indicated this saved an average cost of 400 euro per consultation compared to the physical consultation.
Also the point of possible overuse of the public system, or the fear of a high amount of referrals was tackled early on. A 1999 study with oftalmology patients showed 23 out of 24 patients could be helped by videoconsultation. Estimations were that 21 had needed referral to a specialised clinic whithout the possibily of teleconsultation in place. Now only 6 patients needed the referral.
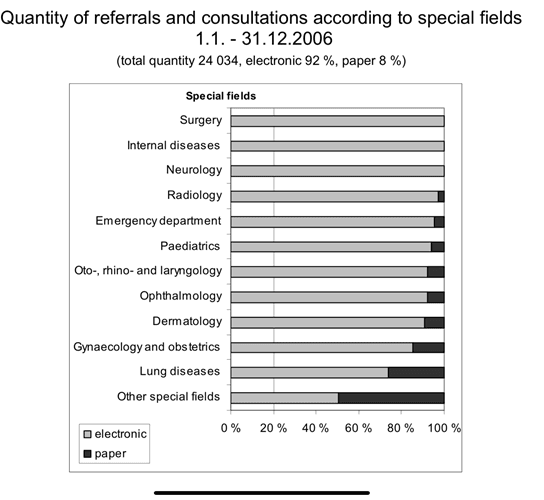
A well-known study of Timonen in 2004 estimated that 3 out of 4 from a random population in general practice could be treated in teleconsultation. Of course, not all doctors wanted this. But even at that time already, surveys showed patients valued teleconsultations the same as physical consultations. Both patients and Health Care Workers (HCW) preferred video consultations before referrals to classical consultations. There was no difference in the number of repeat visits.
In 2015, The National Supervisory Authority for Welfare and Health (VALVIRA) approved online health services by means of a video consultation or smartphone. VALVIRA assigned a set of rules for online HC services by all HC providers. They include data protection and cyber security, patient safety and the proper training of the healthcare professionals delivering online care.
This opened the way to telehealth in primary care, the first contact point for all patients.
Telehealth in primary care in Finland
The cost for a videoconsultation is the same as the cost for a traditional appointment. Increased rates for the weekend are applied. In addition to the appointment fee, an outpatient clinic fee (22,80 EUR) and a Kanta fee (2,10 EUR) are charged. The service is free of charge for occupational health care customers, if it’s included in their company’s occupational health care contract. The duration of an average online consulation is less then 12 minutes.
The most common reasons for consulting the online physician are:
- acute respiratory symptoms (cough, sore throat, fever, running nose),
- “red eye”
- urinary tract infections
- allergies and skin manifestations
- prescription renewal
- family planning and birth control
- sexually transmitted diseases
- mental health and traumatic experiences
- headaches and migraines.
We know this is about the same in other European countries: telehealth works fine for most of the primary care ‘simple’ symptoms.
For Finnish physicians it soon became clear that treating certain medical conditions was made possible without compromising high standards of quality, ethics and patient safety. Videoconsultation made it possible to create their working days with maximal flexibility to working life. Plus: the example of Terveystalo (see below) illustrated soon digital consultations can help as many patients on 1 day as does a traditional health centre with 15 to 20 full-time time physicians. It’s clear this helps to solve the need for HCP all countries face nowadays and which is not expected to diminish.
But although 89% of Finnish people were using the internet in 2018, the use of diverse telehealth services remained rather limited. In 2014, ‘only’ 12% of all citizens reported to have used one or more telehealth services. According to Hypponen et al. (2015) this has a lot to do with low user-friendliness of the terms of use and accessibility conditions in the public system. The challenge of Finnish healthcare digitization is to make the e-services more user-friendly for both patients and professionals.
This is where private telehealth companies come in. They offer stand alone services or work as a contractor for public health centres in Finland.
Terveystalo, Medics24 and Mehilainen digital clinic offer hybrid care in Finland
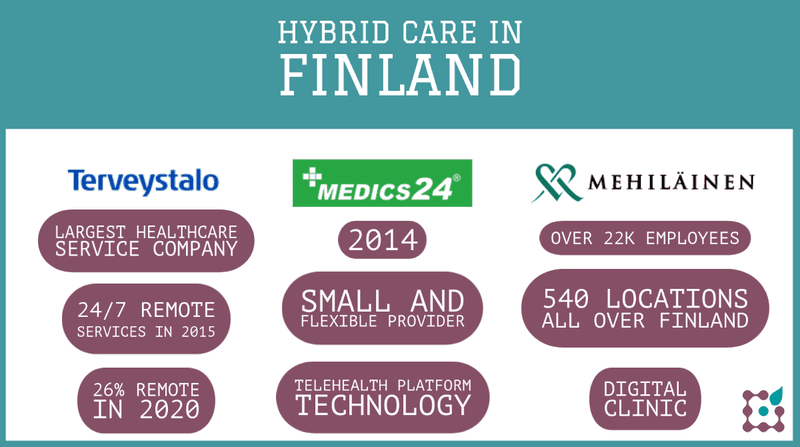
Terveystalo is the largest healthcare service company in Finland and since 2017, it’s noted on Nasdaq Helsinki’s main list. They offer versatile healthcare, occupational healthcare, medical and examination services in 300 clinics all over Finland and via 24/7 telehealth service. Customers include private individuals, companies and communities, insurance companies and the public sector.
They were one of the first to start with 24/7 remote services in 2015. Video appointments are offered by GPs, specialists, psychologists, dietitians and nurses. The physicians are private practitioners and pick patients from a virtual queue. They are mostly experienced professionals who are comfortable with their clinical skills and decision-making. All the online physicians form a virtual community, with the ability to consult one another, discuss various topics and create a sense of common target – to deliver high quality medical care in a new environment. In 2020, 26% of all consultations at Terveystalo were remote: 1,8 million digital visits.
Medics 24 was founded by Tero Nyman in 2014, after a terrible HC-service experience with his daughter: it took 4 hours to see a doctor, of which only 5 minutes for the patient-doctor contact. It’s a small and flexible provider, working with independent physicians, nurses and specialists offering chat or videoconsultation. They cooperate, inter alia, with Ylismedi, a regional private health centre and with Finn Health, ‘the most modern hospital in Finland’ and ‘providing a superior Finnish experience of health’. M24 connect is also part of this group, delivering the telehealth platform technology for diverse health care workers.
A third Finnish provider of hybrid care is Mehilainen digital clinic: it has 540 locations all over Finland, offering occupational, primary and specialist care and social services. it has over 22k employees and private practitioners. Digital clinic is an important and growing part of the group: Mehilainen recently invested in new developments towards integrated telemedicine services (with Beehealthy), and digital consultations are less expensive for patients than physical ones.
- Join +2000 health innovators
What will the future bring?
At the outbreak of the pandemic, Finland benefited from its experience. It rapidly expanded the use of telemedicine for urgent and nonurgent visits. The result: today, 53% of the Finnish people use virtual care and 37% of all healthcare professionals do.
The future of Finlands’ telehealth seems bright. Within the coming decade, Finnish healthcare professionals will have unhindered access to data and information needed in routine healthcare practice, thanks to their focus and experience with health data. Telemedicine applications will abound for consultations with other professionals and patients. Teleconsultation of one’s own treating clinicians will be routinely available and hybrid care will be a commodity for all.
Recently, Finnish telehealth providers go international and cooperate to build better measurement tools and an IoT of mobile health devices for teleconsultations. This will make efficiency and accuracy even better.
These kinds of service innovations would be game changers. They save face to face time for those most in need. The new way for a physician to organise the working days and being part of the online community creates an unprecedented flexibility to working life. Of course, ethical and patient safety issues moust be closely considered. Several issues must be taken into account, like data privacy, cyber security, training the physicians, collecting feedback from both the physicians and the patients is of essence in continuous improvement.
Thanks to Wouter DC for the co-authorship of this article.
1.National Institute for Health and Welfare. Official statistics of Finland; 10.01.2019.
Feel free also to check this out: our best blogs on telehealth all in one place now.
OR join the dashplus community to receive FREE two-weekly updates on trends, tools and tips for your work :